A physical airway obstruction produces breathing pauses that characterize sleep apnea. This obstruction could be a larger tongue, huge tonsils or adenoids, a limp soft palate, or even a deviated nasal septum.
These blockages halt breathing, causing the body to fear and partially wake up to restore regular respiration and need to use sleep apnea machine. These apneic episodes can occur up to 100 times each hour in the most severe instances! Since all these occur when you’re unconscious, how can you tell if you have sleep apnea?
Related: Curing Pediatric Sleep Apnea
Diagnosing Sleep Apnea
Your doctor may assess your symptoms, which you can offer with the assistance of someone who shares your bed or household, if possible. A doctor will almost certainly refer you to a sleep disorder facility. A sleep specialist can assist you in determining whether you require additional evaluation.
An evaluation frequently includes monitoring your breathing and other physiological systems while sleeping at a sleep clinic. Home sleep testing may also be an option.

The following tests are used to detect sleep apnea:
- Polysomnography during the night: You are linked to equipment that measures your heart, lung, and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep throughout this test.
- Sleep tests at home: Your doctor may give you simple tests to perform at home to diagnose sleep apnea. These tests often take your heart rate, blood oxygen level, airflow, and breathing patterns into account.
If the results are abnormal, your doctor may be able to recommend treatment without requiring additional testing. However, because portable monitoring equipment does not detect all types of sleep apnea, your doctor may recommend polysomnography even if your initial results are normal.
To investigate the causes of central sleep apnea, you may require a doctor who specializes in the heart (cardiologist) or a specialist who specializes in the nerve system (neurologist). If you have obstructive sleep apnea, your doctor may recommend you to an ear, nose, and throat specialist to rule out nasal or throat blockage.

Treating Sleep Apnea
To combat this illness, your doctor may merely recommend lifestyle modifications, such as decreasing weight or quitting smoking, for milder forms of sleep apnea. If you have nasal allergies, your doctor will advise you on how to treat them.
If these methods do not help your symptoms, or if your apnea is moderate to severe, a variety of alternative therapies are available.
Certain devices can aid in the opening of a clogged airway. However, a patient may require surgery in some circumstances.
SLEEP APNEA THERAPIES
Continuous Positive Airway Pressure (CPAP)
If you have moderate to severe sleep apnea, a machine that supplies air pressure through a mask while you sleep may be beneficial. The air pressure provided by CPAP (SEE-pap) is slightly higher than that of the surrounding air and is just enough to keep your upper airway passages open, preventing apnea and snoring.
Although CPAP is the most frequent and reliable technique for treating sleep apnea, it can be difficult or uncomfortable for some people. Some people abandon the CPAP machine, but most people learn to adjust the tension of the straps on the mask to get a comfortable and secure fit with practice.
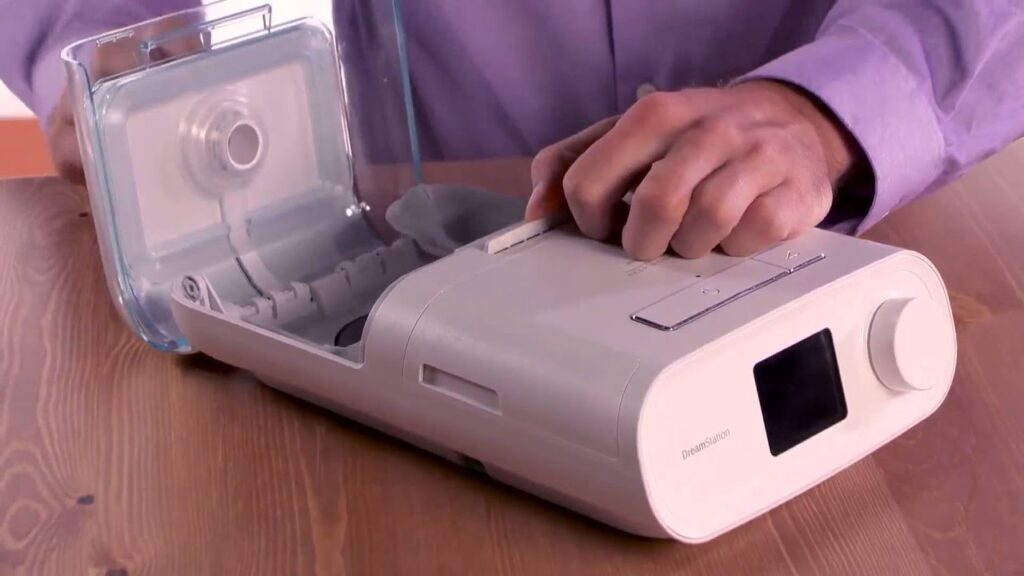
To locate a comfortable mask, you may need to try many different types to locate a comfortable mask. If you experience troubles, don’t stop using the CPAP machine. Consult your doctor to determine what modifications you need to improve your comfort.
If your weight changes, the CPAP machine’s pressure settings may need to be modified. However, contact your doctor if you are still snoring or if you start snoring again despite treatment.
Adaptive Servo-Ventilation (ASV)
This newly certified airflow device learns your typical breathing pattern and stores it in a built-in computer. After falling asleep, the machine applies pressure to restore your breathing rhythm and prevent breathing pauses.
In certain cases, ASV appears to be more effective than other forms of positive airway pressure in treating complicated sleep apnea. However, it may not be a good option for patients with severe central sleep apnea and advanced heart failure.
You’ll probably read, hear, or see TV commercials for various sleep apnea treatments. Before attempting any treatment, consult with your doctor.
Other Airway Pressure Monitors
If using a CPAP machine proves to be an issue for you, you may be able to utilize a different type of airway pressure device that regulates the pressure automatically while you sleep (auto-CPAP). Some units provide bilevel positive airway pressure (BPAP). Oral appliances produce more pressure when inhaling and less pressure when exhaling. Wearing an oral appliance designed to keep your throat open is another possibility. Although CPAP is more reliable than oral equipment, oral appliances may be easier to use. Some help to open your throat by pushing your jaw forward, which can help with snoring and moderate obstructive sleep apnea.
Your dentist can provide you with various equipment, or you can check out some of the equipment listed here. You may need to experiment with many gadgets before finding one that works.
Once you’ve found the proper fit, you’ll need to see your dentist frequently during the first year and then regularly to check that the fit is still good and reassess your indications and symptoms.
Surgery
Surgery is normally reserved for when all other therapies have failed. Before considering surgery, you should try other therapy options for at least three months. However, it is a good first option for a small percentage of people who have particular jaw structure abnormalities.
Surgical alternatives could include:
- Tissue extraction
- Shrinkage of tissue
- Repositioning of the jaw
- Implants
- Stimulation of the nerves
- Tracheostomy
- Surgical removal of swollen tonsils or adenoids
- Bariatric (weight-loss) surgery
Nasal Masks
With this device, the air pressure is supplied through the nose mask. It could be beneficial if:
- Your doctor has advised you to use a high air pressure setting.
- In your sleep, you move a lot.
Home Remedies and Lifestyle Adjustment
Self-care may help you deal with obstructive sleep apnea and potentially central sleep apnea in some circumstances. Consider the following suggestions:
- Exercise: Even without losing weight, regular exercise can help alleviate the symptoms of obstructive sleep apnea. Most days of the week, try to get 30 minutes of moderate activity, such as a brisk walk.
- Avoid alcohol, tranquilizers, and sleeping pills: These loosen the muscles in the back of your throat, making breathing difficult.
- Get rid of unwanted weight: Even a small weight decrease may help reduce throat congestion. Sleep apnea may disappear in some situations if you return to a healthy weight, but it may reoccur if you gain weight.
- Sleep on your side or abdomen: When you sleep on your back, your tongue and soft palate might lay against the back of your throat, obstructing your airway. Attach a tennis ball to the back of your pajama top to prevent rolling onto your back while sleeping. There are also commercially available devices that vibrate when you sleep on your back.
- Avoid smoking: If you smoke, search for resources to assist you in quitting.
- Avoid medicines that make you sleepy.
- Do not drink four to six hours before going to bed.
- Avoid driving if you are drowsy.





